Root canal therapy fits under the special dentistry area known as endodontics. Endodontics literally means dentistry within the tooth itself. The procedure treats disorders of the pulp (the soft tissue inside the crown and roots made up of blood vessels, nerves and lymph vessels that help keep your tooth nourished). Endodontic treatment restores your tooth to a comfortable state by removing the damaged tissue and replacing it with a substance that will help preserve the function of the tooth.
There are many reasons that a root canal may be needed but the most common cause is the carious process of tooth decay). When tooth decay begins, it penetrates the outer layer of enamel and creates a cavity. If that process is not stopped, the decay will continue toward the nerve of the tooth. Other causes include a fracture that exposes the pulp, traumatic injury such as a blow to a tooth, a cracked or loose filling or repeated fillings in a tooth and occasionally from periodontal (gum) disease. Regardless of the initial cause, the tooth pulp becomes irritated and an abscess (infection) can occur. Bacteria from your saliva grow within the tooth pulp, causing pressure and pain. Eventually the pulp dies, causing the bone around the tooth to be destroyed.
All dentists receive some training in endodontic therapy, however, you may be referred to an endodontic therapy, however, you may be referred to an endodontist, a specialist who limits his/her practice to root canal procedures. The sooner you get treatment the better: your risk of losing the damaged tooth is decreased, your pain can be relieved, and your dentist may prevent infection from spreading further.
If you learn how healthy teeth can become damaged, you will understand why root canal therapy may be the best treatment to restore your mouth to a healthy state.
An outer enamel layer and the dentin inside protect the tooth’s underlying structures and prevent bacteria from entering the tooth.
The pulp helps nourish the tooth via blood and lymph vessels that carry nutrients and waste to and from the tooth, and gives the tooth feeling via the nerves.
The root canals house the pulp and extends to the underlying bone.
The bone holds the tooth with the help of tiny periodontal ligaments attached to the roots. The pulp tissue enters and exits through openings at the root tips.
Bacteria can invade your tooth through a loose filling, a cavity, or a crack.
Your pulp becomes inflamed and infected as it is attacked by bacteria. Eventually, the bacteria may destroy the pulp.
The inflammation and infection spread down the root canal, often causing sensitivity to hot or cold foods, throbbing, aching, or pain when you chew.
Your bone may become infected and abscessed as the bacteria escapes though the root openings the bone breaks down, and your periodontal ligaments may swell and loosen your tooth.
Once it has been determined (with x-rays and clinical examination) that root canal treatment is necessary, you will be scheduled for one or more appointments. Your visits may last one to two hours, and you may receive local anesthesia. A rubber dam (a protective sheet of rubber that covers your mouth) may be used to isolate your tooth and prevent bacteria from entering it. The goal of the root canal therapy is to improve the health of your damaged tooth by removing the pulp from your root canals through a small opening in the crown. Then the canals are sealed with special materials to prevent bacteria from reaching your bone. Your dentist then restores the outside of your tooth so it will function properly and have a healthy appearance. After root canal therapy, your tooth continues to be nourished by your surrounding gums and bone.
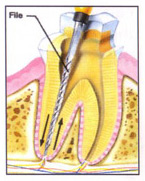
First, your dentist makes an opening in your tooth, and removes any filling and decay. Then, the unhealthy pulp is removed with tiny, flexible files. By using delicate, up-and-down motions, your dentist gently cleans and smooths your canals to prepare them for the canal-filling materials.
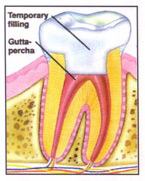
After the pulp has been removed from your root canals and they have been smoothed, your dentist may fill the canals with tiny cone-shaped pieces of gutta-percha, a firm, rubberlike material, or use another dental material. A sealer- cement is used to seal the filling material into place.
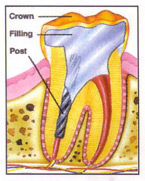
After the inside of your tooth has been treated the outside will be restored to protect your tooth’s underlying structures and to give it a healthy appearance. If your tooth needs extra support, some of the gutta-percha may be removed and a post inserted before the filling and crown are applied.
Once the root canal treatment has been completed, you should be aware of the following considerations:
Discolouration: occasionally an endodontically treated tooth may undergo a change in colour. While this is of no great medical concern, you may be interested in having the tooth bleached. Be sure to ask your dentist about tooth bleaching.
Brittleness: a non-vital (endodontically treated) tooth is more brittle than a vital one, and is more susceptible to fracture. Therefore, we recommend that your root canal teeth be crowned (capped) following treatment.
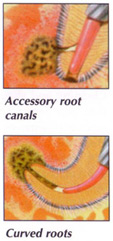
Occasionally a tooth that has undergone endodontic treatment fails to heal or pain continues despite therapy. Some of the special complications that can occur include accessory root canals (large side canals coming off the main canal that cannot be cleaned out), badly curved or cracked roots and narrow canals that prevent thorough cleaning and sealing of the damaged tooth. Sometimes, for unknown reasons, tissues simply fail to heal or a tooth that initially responds to root canal therapy becomes painful or diseased therapy becomes painful or diseased months or years later.
Despite the cause, retreatment may be necessary to save the tooth. During retreatment, the tooth is reopened and the canals are cleaned, filled and sealed again. There are, of course, no guarantees that the procedure will be successful but your endodontist can discuss with you the chances of success before the tooth is retreated. Extraction is the only alternative to retreatment and unless the tooth is replaced with an artificial one (an expensive procedure), adjoining teeth will shift, interfering with biting and chewing. Loss of a tooth can also lead to periodontal disease and loss of additional teeth.